

If you struggle with constant tiredness, brain fog, unexplained weight gain, constipation, feeling cold all the time, or changes to your hair, skin, and nails, and think your thyroid might be to blame, don't rush into iodine therapy. Not all thyroid treatments are created equal, and we want to shed some light on why iodine therapy could be doing your thyroid health more harm than good.
Could Iodine Therapy Be Making Your Thyroid Disease Worse?
You have probably heard of the Dirty Dozen food list, but did you know that this list is updated each year? If you want to be more conscious about the foods you put into your body or have concerns about pesticide contamination, here’s what you need to know before heading to the grocery store so you can make more informed choices:
The Dirty Dozen List: Popular Produce Full of Pesticides
Have you received the diagnosis of a positive ANA (antinuclear antibodies) and then…nothing happened? Perhaps your doctor mentioned something along the lines of, “We will keep monitoring it,” or “Let’s check again in a few months." And there you are, dealing with life-altering symptoms such as brain fog, relentless fatigue, unresolved joint pain, and growing frustration. So what are your options? Are you expected to simply wait for the inevitable crash and burn? Keep reading to learn more about why a positive ANA test is not an invitation to ‘wait and see’.
What A Positive ANA Test Really Means: It’s Time to Dig Deeper
Do you often find yourself unbuttoning your pants after a large meal and blaming your bloating on eating too fast or overeating? Common symptoms such as gas and bloating after meals can often be brushed under the rug as just one of those unavoidable or random parts of being human, and not something that should be addressed. So what if these post-meal symptoms– bloating, gas, brain fog, fatigue, etc. aren’t really “normal” at all?
Are Gas and Bloating After Meals Normal? What Your Gut Might Be Telling You
Have you ever looked at your blood test results and noticed that something referred to as "ferritin" was elevated? Perhaps your primary care physician disregarded it, or even worse, never mentioned anything about it. High ferritin levels are actually extremely important and could be connected to inflammation in the body, so read on to find out why you shouldn’t ignore this iron marker in your bloodwork!
What Do High Ferritin Levels Really Mean?
Could your birth control be messing with your thyroid? If you’re a woman who’s been on birth control for years, it’s important that you know about the potential long-term effects. We want to raise awareness about the link between birth control and hypothyroidism so that you can ask the right questions and advocate for your health. Because the research (and clinical experience) is showing us something big: Long-term birth control use may significantly increase your risk of developing hypothyroidism.
Birth Control and Hypothyroidism: What Every Woman Needs to Know
So, you’ve just been diagnosed with Hashimoto’s thyroiditis and you're wondering...What now? You’re not alone—and more importantly, you're not stuck. Let's break it down together!
What Do I Do Now That I Have Hashimoto’s?
Do you consistently reach for Benadryl to help with allergies or get a better night's sleep? You are not alone, as it is a common and easily accessible over-the-counter medication, but did you know that long-term use of antihistamines like Benadryl could have serious consequences for your brain health? We want to share some of the lesser-known risks and things you should be aware of about long-term antihistamine use.
The Hidden Danger of Long-Term Antihistamine Use
Do you often feel lightheaded or experience dizziness? Perhaps even deal with migraines, extreme fatigue, or fainting episodes. These symptoms can be very confusing and bewildering, frequently being misdiagnosed as anxiety or other neurological disorders. However, there is a lesser-known condition that can cause all of these symptoms, known as Postural Orthostatic Tachycardia Syndrome, or POTS for short.
POTS: The Mysterious Condition Behind Dizziness, Brain Fog & More
Do you feel like Mom or Dad is starting to show signs of “losing it”? Perhaps they’re struggling more than normal with basic tasks, experiencing memory slips, or unable to think clearly. And while you’d probably dismiss it as normal aging, the truth is, there could be something else at play that’s worth digging into. We want to shed some light on a much more nuanced explanation, and no, it’s not simply a case of mental health deterioration. It might be their blood sugar. Yes, the same issues that induce diabetes are one of the leading causes of dementia in the U.S.
Blood Sugar, Dementia & the B12 Connection: What to Know if Mom or Dad Is "Losing Their Mind"
Do you feel like you’re battling never-ending fatigue, confusion, and frustration? Perhaps you’re plagued with insomnia, depression, anxiety, joint pain, chronic fatigue, or brain fog with no relief for years. Although you know something is off, it seems no one has the answers. Does this resonate with you? If so, you are not alone. The critical missing piece to the puzzle is often comprehensive blood work.
Comprehensive Blood Work: The Missing Piece in Your Health Journey
Have you been diagnosed with the MTHFR gene mutation? Then you need to know about its connection to B vitamins! Methylated B vitamins are important in maintaining your health living with the MTHFR gene, but they’re not always found in common supplement brands. But what makes methylated vitamins better? Read on to learn more!
The Importance of Methylated B Vitamins & Why You Should Care
Here at Dr. Autoimmune, we dig deep into potential causes of leaky gut and other autoimmune conditions to better understand the factors causing your symptoms. One of the first stages of autoimmunity can often be dysbiosis which isn’t always detected in regular bloodwork, which is why early detection is key to preventing disease progression. We look at over 85 different blood markers that traditional doctors don’t test for, ensuring that we have the best overall picture, so keep reading to learn more about dysbiosis and how it affects autoimmunity.
A Guide to Dysbiosis & Autoimmunity
Did you know that magnesium plays a role in proper immune T-cell function as well as impacts inflammation, one of the hallmarks of autoimmunity? This powerful mineral is not to be overlooked, as its positive effects on immune health and inflammatory response are significant. Here are some important things to know about the benefits of taking magnesium:
The Benefits of Taking Magnesium
Autoimmunity can manifest in a variety of ways, with symptoms that come and go, frustrating gut issues, and chronic pain that impacts your day-to-day life, not to mention brain fog, sleep disorders, and more. This is why misdiagnosing can be a common problem and finding ways to manage your condition is even harder. With more and more research being done about potential root causes of chronic conditions like POTS, the link between it and autoimmunity is growing stronger, which helps our holistic specialists know how to help patients find relief from their symptoms. Read on to learn more about the connections between POTS and autoimmune disease:
The Connection Between POTS And Autoimmunity
Extra virgin olive oil (EVOO) is the highest quality olive oil made from the fresh juice of the olive without the use of chemicals or heat. This cold-pressed method results in a darker, more flavorful product that provides substantial benefits for autoimmunity and inflammation. EVOO is a staple in the autoimmune protocol diet, so keep reading to learn more about olive oil benefits; plus, find out which olive oil is the best and why!
Olive Oil Benefits: Is It a Food or a Supplement?
Holiday gatherings typically center around food, and if you’re on the AIP diet, then navigating your food choices can sometimes be difficult. That’s why we want to share some of our best tips for maintaining your autoimmune protocol during the holiday season, as well as several Thanksgiving AIP recipes!
Our AIP Diet Guide and How to Successfully Navigate the Holidays
The thyroid is a butterfly-shaped organ in your neck, and although it’s relatively small, it has a pretty big role in major processes throughout the body. It communicates with the brain, releases hormones that regulate heart rate, body temperature, and more, as well as supports sleep, immune function, and digestion. Thyroid diseases such as Hashimoto’s are common chronic illnesses that result in hormone imbalances and debilitating symptoms that can also aggravate autoimmune activity in other areas of the body. So what is Hashimoto’s disease? Read on to learn more about causes, symptoms, effects on nutrition, and how to improve your thyroid health!
What is Hashimoto's Disease?
Women are at a much higher risk of iron deficiency, especially menstruating and pregnant women. However, iron level screenings aren’t usually a priority, resulting in many women experiencing unexplained symptoms that lower their quality of life. We want to share the importance of iron, as well as signs of iron deficiency and how to get the most accurate blood panel to test for anemia, so keep reading to learn more!
10 Signs of Iron Deficiency in Women
Collagen is a powerful substance your body needs for a variety of functions, not just for protecting your hair, skin, and nails! From your gut lining to your risk for osteoarthritis and osteoporosis, collagen plays a vital role in your overall health. So keep reading to find out– why is collagen important?
Why is Collagen Important?
Are you skeptical about telemedicine and whether it’s actually beneficial for your health needs? We understand that dealing with a chronic autoimmune condition can be exhausting, going to multiple doctors in various cities without a proper diagnosis or effective solution. That’s why we started Dr. Autoimme, a fully online functional medicine practice! Read on to learn more about how it works!
Answering FAQs About Online Functional Medicine
Lupus affects 1.5 million people in the U.S., and 90% of those are women. Often called “the great imitator”, this chronic illness can initially look like other diseases, and symptoms can even come and go, delaying a correct diagnosis by months or even years. In fact 1 in 3 people living with lupus deal with multiple autoimmune conditions! So, exactly what is lupus and what causes it to wreak havoc on your body? Is there a way to manage it? Keep reading to find out how Dr. Autoimmune helps support lupus patients and find relief!
What is Lupus: Symptoms, Causes & How We Can Help
Known for its anti-aging properties, NAD is commonly used to maintain vitality and boost feelings of wellness. But did you know it has become a beneficial option supporting autoimmunity? From multiple sclerosis and rheumatoid arthritis to type 1 diabetes and Crohn’s disease, NAD is certainly something you should know about. Keep reading to learn more about this tiny and incredible molecule that has a big impact on the body and how NAD for autoimmune disease can benefit you!
6 Things to Know About NAD for Autoimmune Disease
Autoimmune disease affects men and women of all ages, and it can be overwhelming to know where to start when it comes to finding the right solution for your symptoms. Whether you are experiencing early signs of an autoimmune disease or have been dealing with a chronic condition for years, learn more about our “do it yourself” 3o-day reset program that has helped many people restore optimal health!
A Complete Guide to our DIY 30-Day Reset Program
Are you tired of juggling prescription medications with side effects worse than your symptoms or frustrated with not getting answers about what is causing your symptoms in the first place? You need to get help from Dr. Autoimmune! We offer a unique holistic approach to autoimmune disease and functional medicine, ensuring your body can heal itself with the help of meaningful lifestyle changes, nutrition, supplementation, and other natural therapies.
What to Expect From our Holistic Approach to Autoimmune Disease
You may be familiar with N-Acetylcysteine as a prescription medication used to treat acetaminophen overdoses as well as certain chronic lung conditions, but it is also available as an over-the-counter supplement with many potential benefits for those living with an autoimmune disease. In fact, it’s so good that there has been an attempt by the FDA to ban it! So if you’re wondering, “What is N-Acetylcysteine?”, then keep reading because we want to share with you the power of a little amino acid known as NAC.
What is N-Acetylcysteine (NAC)?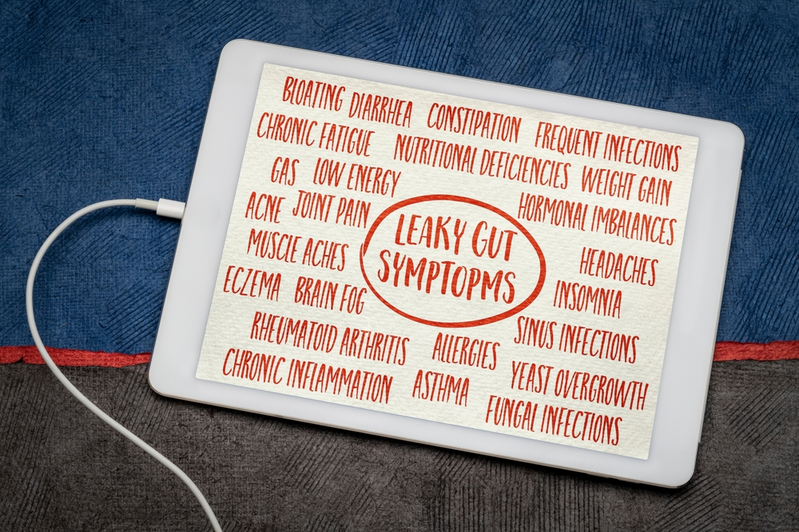
We support a wide range of chronic autoimmune conditions, from inflammatory bowel disease to Sjogren’s Syndrome. Many, if not all, originate in the gut, and leaky gut syndrome contributes to worsening autoimmune symptoms. Read on to learn more about the signs of leaky gut syndrome and how our autoimmune specialists help find solutions so that you can reach your health goals.
7 Signs of Leaky Gut Syndrome & What to Do Next
One of the symptoms of low thyroid is weight gain or the inability to lose weight, often caused by a slowed metabolism. This isn’t the only autoimmune condition that affects your metabolism, so we have become experts at identifying the root causes of your digestive and energy problems so that you can start seeing some improvements in how you feel on a daily basis. Keep reading to explore how to improve your metabolism naturally!
How to Improve Your Metabolism Naturally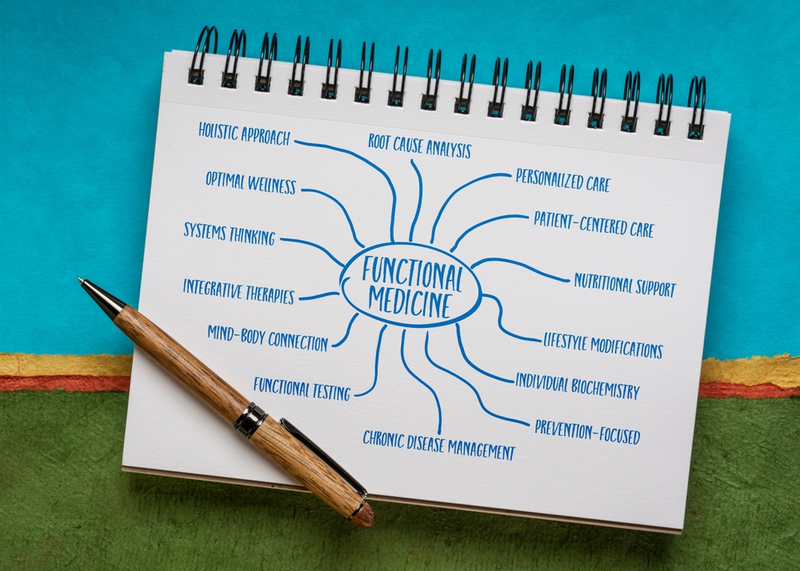
At our functional medical center, we firmly believe that healthcare is specific to the individual and requires attention to detail and personalized care plans. We also know that our bodies are capable of healing themselves. These are a few core <a href="/the-5-principles-of-functional-medicine/">functional medicine principles</a> our team is passionate about! So, what is functional medicine? Read on to learn more about our holistic approach to health and wellness!
About our Holistic Approach: What is Functional Medicine?
Inflammation is your body’s natural response to harmful toxins, infection, and injury. Your immune system is designed this way to repair damaged cells and begin the healing process, but when you experience long-term inflammation, it can lead to a variety of debilitating issues. We want to discuss the difference between acute and chronic inflammation and how inflammatory balance is key for managing autoimmune conditions.
The Difference Between Acute and Chronic Inflammation
The thyroid gland is responsible for producing hormones that control your energy and metabolism, as well as regulate your body temperature and other system functions. Millions of Americans suffer from thyroid conditions like Hashimoto’s and Graves’ disease, and the majority of the time, it’s an autoimmune-related issue, meaning that your body’s immune system attacks your thyroid. Keep reading to learn more about the early signs and symptoms of low thyroid and what you can do to feel better!
12 Signs and Symptoms of Low Thyroid
Do you want to learn more about your health and how your diet impacts vital functions within your body? Our Clinical Nutritionists work with adults with a variety of health concerns to reach their goals and take control of their well-being. So, what is clinical nutrition? Read on to discover exactly what you need to know about this service, the signs and causes of nutritional deficiencies, and how you could benefit from our holistic approach to overall wellness!
What Is Clinical Nutrition?
Chronic disease affects millions of men and women in the U.S. and often affects nearly every aspect of everyday life. From thyroid issues to leaky gut, autoimmune disorders can be difficult to diagnose and even more tough to treat. Thankfully, the team at Dr. Autoimmune specializes in helping patients find the answers and experience relief. Read on to find out more about our Autoimmune Specialists and how we can best serve you!
5 Things to Know About Our Autoimmune Specialists and How We Can Help
Probiotics are living microorganisms responsible for breaking down and absorbing nutrients, maintaining the immune-gut barrier, and much more. When combined with prebiotics, these healthy bacteria strains encourage a high-functioning immune system and provide relief from frustrating symptoms such as diarrhea, constipation, bloating/gas, and other IBS symptoms. Here are a few benefits of probiotics you should know about:
6 Benefits of Probiotics
As we navigate the complex landscape of COVID-19, scientific exploration continues to uncover intricate links between the virus and various health factors. Recently, a notable study published in the National Center for Biotechnology Information sheds light on a critical aspect—dysbiosis, the imbalance in gut microbiota, as an indicator of poor outcomes in COVID-19 infections.
Unveiling the Connection: Dysbiosis as a Crucial Indicator in Covid-19 Outcomes
In a recent study published in the <a href="https://drknews.com/leaky-gut-autoimmunity-study/" target="_blank" >International Journal of Molecular Sciences</a>, researchers shed light on the profound implications of a compromised intestinal barrier (Intestinal permeability, IP), colloquially known as leaky gut. The groundbreaking findings reveal that individuals with leaky gut face a staggering 30-fold increased likelihood of developing autoimmunity compared to those with a healthy gut.
Unlocking the Secrets of Leaky Gut: Study Reveals 30x Increase in Autoimmunity!
In the intricate web of the human body, the gut plays a pivotal role in maintaining overall health. However, when the delicate balance within the digestive system is disrupted, it can lead to a condition known as Leaky Gut Syndrome. This phenomenon occurs when the intestinal barrier becomes compromised, allowing undigested particles and toxins to pass into the bloodstream, triggering inflammation and a cascade of health issues. Let’s delve into the seven mechanisms contributing to Leaky Gut and explore how Dr. Autoimmune’s functional medicine approach provides a beacon of hope for those seeking relief.
Unveiling the 7 Mechanisms of Leaky Gut
A well-balanced diet that includes foods rich in the nutrients mentioned above can help manage Hashimoto’s. Additionally, some people find relief from symptoms by eliminating gluten, as it can exacerbate inflammation and autoimmunity in some cases. A diet high in fruits, vegetables, and whole grains can provide essential nutrients and fiber to support overall health.
Nutritional Deficiencies in Hashimoto’s: Understanding, Prevention, & Support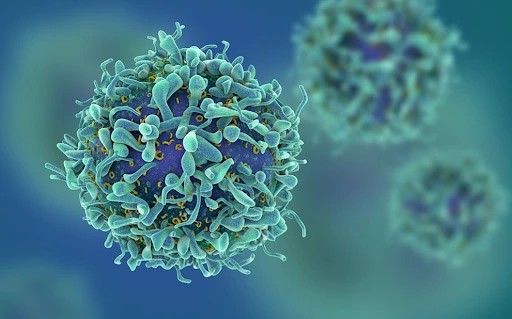
Autoimmunity is a condition where the immune system mistakenly targets and attacks the body’s own tissues and cells. It can lead to a range of debilitating diseases, such as rheumatoid arthritis, multiple sclerosis, and lupus. Regulatory T cells (Treg are a crucial component of the immune system responsible for maintaining self-tolerance and suppressing autoimmune responses. In this blog, we will explore the significance of Treg cells in the context of autoimmunity and discuss how dietary factors like green tea, probiotics, and high-fiber diets can influence their function.
The Role of Regulatory T Cells in Autoimmunity
The COVID-19 pandemic, caused by the novel coronavirus SARS-CoV-2, has upended lives worldwide since its emergence in late 2019. Initially regarded as primarily a respiratory illness, it has become increasingly evident that COVID-19 can affect various systems in the body, including the gastrointestinal (GI) tract. In this blog post, we delve into how COVID-19 infections raise the risk of gastrointestinal problems, explore the symptoms and complications, and shed light on how functional medicine and supplementation can aid in addressing residual gut issues stemming from COVID-19.
Unmasking the Link Between COVID-19 and Gut Issues
In the intricate world of the human immune system, maintaining a delicate balance is crucial to prevent autoimmune diseases and other immune-related disorders.
Boosting Immunity: Prebiotics & Treg Cells
In recent years, the concept of intestinal <a href="/what-is-leaky-gut/">hyperpermeability</a>, more commonly known as “leaky gut,” has gained significant attention in the realm of health and wellness. Leaky gut refers to a condition where the intestinal lining becomes compromised, allowing toxins, undigested food particles, and bacteria to leak into the bloodstream, triggering a cascade of inflammatory responses and contributing to various health issues. However, amidst this concern, a remarkable natural remedy has emerged – <a href="https://www.naturalmedicinejournal.com/journal/nutrient-profile-zinc-carnosine#:~:text=Summary-,Zinc%2Dcarnosine%20is%20a%20unique%20product%20that%20appears%20to%20enhance,pylori." target="_blank" >Zinc Carnosine</a>. In this blog we’ll be going over this unique compound in how it not only aids in healing leaky gut, but also how it possesses a vast array of healing capabilities for the whole body.
The Power of Zinc Carnosine: Healing Intestinal Hyperpermeability and Beyond
The intricate relationship between gut health and autoimmune diseases has garnered significant attention in recent years. Scientific studies have unveiled the impact of a healthy gut on the immune system, revealing how imbalances in the gut microbiome can contribute to the development and progression of autoimmune disorders. In this blog post, we will delve into the connection between gut health and autoimmune disease, explore the symptoms, discuss the role of probiotics and supplements, and shed light on the autoimmune diet for gut repair. Furthermore, we will highlight how functional medicine practitioners like Dr. Autoimmune can play a crucial role in treating gut problems associated with autoimmune diseases.
The Connection Between Gut Health and Autoimmune Disease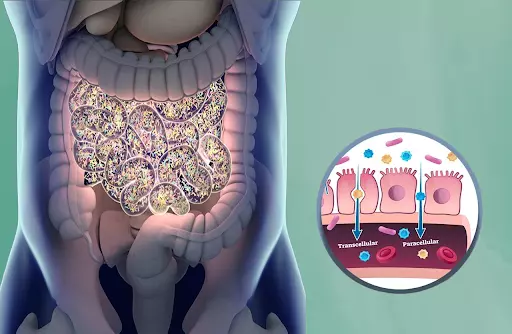
In recent years, there has been a growing interest in the connection between gut health and various autoimmune conditions. Two conditions that have gained attention are leaky gut and Sjogren’s disease. Although they share some similarities, they are distinct in their origins and effects on the body. This blog post aims to shed light on leaky gut and Sjogren’s disease, highlighting their differences and similarities and explore how functional medicine can play a role in managing the associated symptoms.
Understanding Leaky Gut and Sjogren’s Disease
Before delving into the necessary nutrients, it is crucial to understand the basics of thyroid disease. The thyroid gland plays a vital role in regulating metabolism, energy levels, and hormone production. Imbalances in thyroid hormones, such as hypothyroidism, can have a profound impact on overall health.
Necessary Nutrients for Thyroid Disease: Zinc, Selenium & Vitamin D
Gluten has become a buzzword in recent years, often associated with a range of health concerns. But what exactly is gluten, and what are the differences between celiac disease, gluten allergy, and gluten sensitivity? In this blog, we will delve into the intricacies of gluten-related disorders, shed light on the unique challenges they pose, and explore how Dr. Ian Hollaman aka Dr. Autoimmune, a renowned functional medicine practitioner, and his team can offer support and guidance in managing celiac disease, gluten allergies, and sensitivities.
Understanding Gluten: Celiac Disease, Allergy, Sensitivity, and Dr. Autoimmune’s Approach to Healing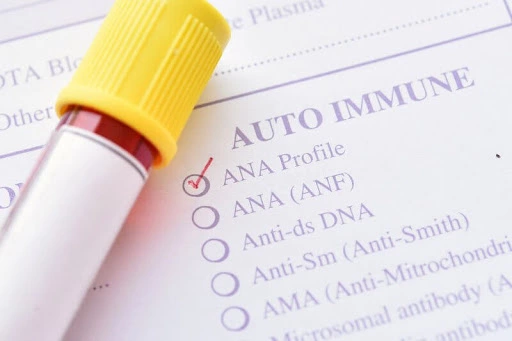
ANA is a group of antibodies that target components within the cell nucleus. This blog aims to provide a comprehensive understanding of ANA and shed light on the various patterns observed, including speckled, nucleolar, and homogeneous patterns, and their clinical significance.
Understanding Lupus and Vasculitis Conditions: Decoding ANA Patterns
Arthritis is a broad term used to describe inflammation and stiffness in the joints, affecting millions of people worldwide. It encompasses various types of arthritis, including seropositive and seronegative arthritis. These terms refer to the presence or absence of certain antibodies in the blood associated with the condition.
Seropositive versus Seronegative Arthritis: Understanding the Differences and Similarities
There are more than 80 different types of autoimmune diseases — diseases, and fifty million Americans alone suffer from an autoimmune disease. So why does this happen? One reason is people with autoimmune disease have too much inflammation in their bodies and they don’t make enough glutathione.
Glutathione & Autoimmune Disease Connection
For a long time we’ve known that bacteria can trigger the immune system in such a way that autoimmune diseases are formed.
Autoimmune Diseases & Infections
Instead of trying to identify which medication will treat your symptoms, functional medicine providers focus on finding the root cause of your issues to restore optimal function and wellness.
Why You Should Consider Functional Care
Childhood may hold some of the best times of our lives, and though much of childhood might seem carefree, when you add an autoimmune disorder into the equation, things tend to get a bit complicated – and scary – for both the child and the parent.
Autoimmune Diseases In Children
Have you got dry skin that seems to need a ton of moisturizer to stop it from cracking and flaking? There can be a few factors involved in causing dry skin but sometimes, it can be linked to autoimmune disease.
Could Your Dry Skin Be a Sign of Autoimmune Disease?
While autoimmune conditions vary widely in symptoms and severity, they all have the same underlying problem: Your body’s immune cells attack your own body.
Is Your Autoimmune Disease Caused By Environmental Factors?
There are a lot of different methods out there that encompass “alternative” medicine. And one of these methods in particular that has gained a great deal of attention in recent years, is Functional Medicine.
The 5 Principles of Functional Medicine
As if women don’t already go through enough between having a monthly menstrual cycle, experiencing childbirth and going through menopause later in life, now recent studies estimate that about 80% of all patients diagnosed with autoimmune diseases are women. That means it’s important for women to be aware and know what to look out for. That’s why in this article we go over the top 5 most common autoimmune diseases and their symptoms that affect women. Our goal in doing this is to better educate women everywhere so they can seek the care they need and get to the root cause of their symptoms earlier rather than later.
Top 5 Most Common Autoimmune Diseases That Affect Women
It seems discussing a Autoimmune diseases in men is not a topic that is discussed very often. That’s because 80% of all patients diagnosed with autoimmune diseases are women, but the gap is getting smaller. This is why we think it’s important that we take a look at the five most common autoimmune diseases and their symptoms in men.
5 Common Autoimmune Diseases in Men
Breathing techniques are not just for yogis and tree huggers, and have been used for thousands of years in many cultures and practices. Almost everyone who has ever been guided through a meditation practice knows how important the rhythm of breath is. Although encouraged to breathe through our nose, for many, that is easier said than done.
Breathe Your Troubles Away
Eczema care from a functional medicine perspective is all about finding the cause. At Dr. Autoimmune, Dr. Ian Hollaman doesn’t only address his patients’ eczema symptoms; he looks for the root cause of the eczema and fixes it!
How Functional Medicine Can Heal Your Eczema
Digestive issues are becoming more and more common! From bloating to IBS to SIBO and Candida overgrowth, there’s no shortage of people walking into my office hoping for a solution to their GI issues.
Healing Crohn’s Disease With Functional Medicine
Discover the vital role of gut health in immune function and disease prevention. Learn how imbalance in gut microbes, known as 'dysbiosis,' can lead to 'leaky gut' and various health issues, including autoimmune diseases like Crohn’s. At Dr. Autoimmune, our personalized, science-backed approach focuses on restoring gut health naturally to enhance overall well-being.
What is Leaky Gut?
Polycystic ovarian syndrome (PCOS) is one of the most common conditions in reproductive-aged women. It is estimated that 8-13% of all reproductive-aged women have this condition and up to 70% of those women are undiagnosed. People with PCOS have cysts on their ovaries that cause hormonal symptoms such as:
Could Your PCOS Medications “B” the Problem?
Have you heard of the “microbiome”? This is the word for a small ecosystem made up of microorganisms such as bacteria, viruses, and fungi. Everyone has ecosystems like these in their body, such as the gut microbiome, the skin microbiome, and pregnant people even have a placental microbiome inside their uterus. These tiny ecosystems are responsible for generating and absorbing essential nutrients, helping with digestion, and even providing a backbone for your immune system. In fact, 70-80% of your immune cells are in your gut!
Maybe She’s Born With It, Maybe It’s Her Microbes
Juvenile idiopathic arthritis (JIA), formerly known as juvenile rheumatoid arthritis (RA), is joint inflammation in children 16 years of age or younger, lasting for at least 6 weeks. Unlike adult rheumatoid arthritis (RA) that is chronic and can last a lifetime without proper diagnosis or intervention, children usually outgrow JIA. But do they really?
Junior Joint Pain
Diabetes affects 11.3% of people in the US, and 90-95% of those people have type 2 diabetes. What many people may not know, however, is that all forms of diabetes will increase your risk of dementia. Glucose (sugar) is an essential source of energy for your brain, so when your insulin is not metabolizing it in a way that makes it useful, your brain misses out on important fuel. A pre-diabetic state is marked by insulin resistance, which is when your insulin cells can’t use glucose effectively.
Diabetes and Dementia and B12 Deficiency, Oh My!
The skin is the largest organ of your body and will sometimes hint at what’s going on beneath the surface when an individual is suffering from certain autoimmune conditions.
How Autoimmune Diseases Can Affect Your Skin
Discover how eating these foods can get you a healthier gut! We’ve all experienced these symptoms more than we can count! Bloating, constipation, diarrhea, indigestion, and the general feeling of blah.
Achieve A Healthier Gut By Eating These Foods
With autoimmune diseases on the rise in the past few decades, we’ve learned to detect early signs of an autoimmune disease to help fill in the gap about what causes the immune system to attack the body’s own tissues and organs.
6 Early Signs Of An Autoimmune Disease
A fifth of the United States is drinking contaminated water. There are contaminants in municipal drinking water such as heavy metals, pharmaceuticals, and other impurities that can affect your health. Some of these contaminants can lead to serious health problems including cancer, autoimmunity, and birth defects. In addition, many of these contaminants are not removed by standard filtration methods. As a result, it is important to be aware of the potential risks associated with drinking municipal water. There are a number of ways to reduce your exposure to these contaminants, including using a water filter or drinking bottled water. By taking simple steps to protect yourself, you can help reduce your risk of exposure to harmful contaminants.
There Must Be Something in the Water
Eating healthy isn’t always enough. We can eat a variety of organic vegetables, fruits, and meats and still be missing out on the macronutrients that these foods deliver. Poor soil health from overcropping leads to less nutrient-dense foods, and our internal gut health may be missing the “good stuff” that helps us absorb and digest these “healthy” food sources.
You Aren’t Always What You Eat
We’ve all experienced these symptoms more than we can count! Bloating, constipation, diarrhea, indigestion, and the general feeling of blah. That’s a common feeling after eating a large greasy meal. Or indulging in a rich dessert. Or grabbing a bunch of convenience food when you’re running late.
Foods to Eat to Get a Healthier Gut
These itty bitty bugs climb out as cold weather fades. Particularly in woody, adventure-seeking communities like Colorado, people take to the outdoors (and so do the ticks!).
A Ticking Lyme Bomb
Green tea has been used for centuries in Asia for its medicinal properties, and recent research has taught us that it may be an important tool for tackling autoimmunity. The extract from green tea has been shown to support T-regulatory cells, which help to suppress an overactive immune response and reduce inflammation. Sunphenon®, a decaffeinated and highly potent green tea extract, is a key ingredient in our proprietary supplement ImmunoXym that provides these benefits.
ImmunoXym: The Best Way to Get the Benefits of Green Tea
Hypertension, or high blood pressure, is the most common chronic disease in America. People with hypertension are at risk for heart attack, stroke, and kidney damage. Did you know that there is a connection between hypertension and autoimmune disease? Were you aware there are over 400 different causal factors in hypertension?
Hypertension and Autoimmune Disease: What You Need to Know
“The best wealth is health,” said the Roman poet Virgil. You may also have heard, “You can have all of the money in the world, but if you don’t have your health, you have nothing.”
The Link Between Mental Health and Antibiotics
“Antioxidant” is probably a term you have heard before. It is used commonly to refer to health beverage ingredients, so-called ‘superfoods’, and supplements as an anti-aging tool. But what is an antioxidant?
The Immune Power of Antioxidants
Your habits influence your attitude, sleep, food cravings…and autoimmunity. Many of you that suspect you may have an autoimmune condition, or have been diagnosed with one, may in fact have two or more lurking within.
There is nothing “Sweet” about Artificial Sweeteners and Leaky Gut
Autoimmunity is when the body attacks its own tissue and organs. In lupus, any bodily system can be attacked, so there are a wide range of possible symptoms. Some of the most common symptoms include:
Lupus and DHEA: A New Approach
It may be hard to believe, but brushing your teeth can help your joints. All dentists will tell you that your dental health is tied to your physical health, but how seriously do we really take that? Your mouth has its own microbiome, which is the mini ecosystem made up of bacteria and other small life forms, just like your gut and your skin. When any of your microbiomes are out of balance, there will be consequences.
Can You Brush and Floss Your Way to Relieved RA?
Your thyroid is a gland located behind your Adam’s apple. Its job is to produce thyroxine (T4) and triiodothyronine (T3) which are the hormones that control your metabolism. This process of transforming the food you eat into energy can result in (T)erminator-like symptoms where you begin to feel inhuman.
Meet the Master Manipulator: Your Thyroid
Many women with autoimmune diseases experience a lessening of symptoms during their pregnancy, only to relapse after the baby is born. Or, the opposite may happen, where autoimmune disease symptoms worsen during pregnancy. Maybe you have heard of this phenomenon or even experienced it yourself. As we continue to celebrate Mothers’ Day, let’s dive into the ways pregnancy can affect an autoimmune disease.
Why Do I Feel So Good (Or Bad) During Pregnancy?
As comes Spring, so comes the opportunity to reap the rewards of homegrown deliciousness. This time of year is known for awakening all of the human senses. What better time to feel at one with the green spaces around you?
Keep it Fresh
April is Sjögren’s awareness month, so we thought it would be a great time to shed some light on it. Sjögren’s (pronounced show-grens) syndrome is a common autoimmune condition where moisture-secreting glands are attacked. This usually happens first in the eyes and mouth, so dry eyes and mouth are the most common symptoms.
What is Sjögren’s Syndrome?
The virus that shook the world has a few symptoms we all know, such as loss of taste and smell. And by now, most of us have heard of the term “long-COVID”, referring to recovered COVID-19 patients who have symptoms long after they test negative for the virus. Long-COVID symptoms include continued absence of smell and taste, difficulty breathing, fatigue, and brain fog. If you have been struggling with this, there is hope!
Still Can’t Smell or Taste After COVID?
Baldness is the name given to the most common type of hair loss, androgenetic alopecia, genetically caused hair loss. Male pattern baldness typically occurs on the top and front of the head. Female pattern baldness occurs on the top, usually widening at the part. Genetics and stress can exacerbate hair loss, but too often our immune system gets involved, and can be the culprit in the alopecia mystery.
A Hair-Owing Dilemma
Are you ready to overhaul your COVID symptoms? Finding relief at the end of a very long, arduous fight can be resolved with proper diagnostics and support. Getting to the root cause of your aches and pains is just what Dr. Autoimmune ordered.
Long COVID Doesn’t Need to be Exhausting
Raynaud’s phenomenon is a condition that can occur on its own (known as primary Raynaud’s), or it can be a sign of an underlying autoimmune condition (known as secondary Raynaud’s). It is estimated to affect an average of 6.5% of all people (8-10% of women and 3-5% of men) and tends to start showing up between the ages of 15 and 25.
The Many Faces of Raynaud’s Phenomenon
Food is medicine. By providing your body with the correct tools, it has the ability to heal itself. Whether you have a diagnosed autoimmune or thyroid condition, or just want to boost your immune system during these trying times, follow this guide to learn how to use food to your advantage!
Top 7 Foods For Immune Support
Are you on the medical not-so-merry-go-round? Many people with thyroid problems aren’t even aware they are connected to the thyroid. Most medical doctors only test for 1-3 out of the 10 markers required to get a complete picture of the thyroid.
Why You Still Have Thyroid Symptoms
The idea that humans are separate from the natural world is a new one. Humans and nature evolved together, developing and perfecting symbiotic (mutually-beneficial) relationships over 6 million years. Has our recent separation led to an increase in health issues, particularly autoimmunity?
Autoimmunity and the Earth
Antinuclear antibodies (ANAs) are antibodies (proteins that our body creates to fight infections) that are made to attack our own body, or “autoantibodies”. The prefix ‘auto-’ means ‘self’. So, autoantibodies are antibodies against the self, and an autoimmune disease occurs when someone’s immune system is attacking their body using autoantibodies. Examples of autoimmune diseases include multiple sclerosis, Hashimoto's thyroiditis, rheumatoid arthritis, scleroderma, lupus, and many more. Antinuclear antibodies attack the nucleus of our cells, hence their name.
Autoimmunity Is Rising- Have You Been Tested?
Oatmeal, waffles, toast, grits are all loaded with carbohydrates. While not inherently bad, carbs are not a good way to start your day! Once converted to glucose in your body, these foods cause blood sugar spikes, giving you a short burst of energy followed by a “crash”. Repeatedly spiking your blood sugar can also lead to <a href="/hormones-101-part-3-insulin-resistance/">insulin resistance</a>, which can make it hard to manage weight, affect other hormone levels, increase your risk of dementia, and cause more sugar cravings. Unchecked, insulin resistance can develop into type 2 diabetes.
12 Habits to Make Your New Year a Healing One
Nicotinamide adenine dinucleotide (NAD+) is a coenzyme central to metabolism. It contains both NAD+ and NADH. It is an important molecule that is found in our cells and its key functions are to keep our DNA healthy by converting food into energy and to regulate our sleep. It has been referred to as our natural fountain of youth.
Say Yes to NAD — a Nootropic for the New Year
Our brain detoxes and restores when we sleep. If we cut our sleep short, we are interrupting this cycle that is imperative to our health. Other research has shown that people who have short sleeping times have higher levels of beta-amyloid in their brain – which is commonly found in the brains of people who have Alzheimer’s disease.
Can You Sleep Too Much?
As a child, were you covered in pink calamine lotion after proclaiming “it itches?” Did your mom soak you in a bath with oatmeal to soften and dissolve those scabs that came after a bout of chickenpox? Mine did.
A Rude Awakening
Do you experience sugar cravings after meals? Are you prone to becoming ‘hangry’ when you need to eat? These are very common things, but they may actually be a sign of insulin resistance- a common trigger for autoimmune diseases.
Hormones 101 Part 3: Insulin Resistance
Every human body is different in so many ways, but one thing we all have in common is poop! Pooping is something every living creature on this planet must do in order to stay alive and healthy. The process of defecation means the discharge of feces from the body. Poop is the left-over waste in our system after all of the nutrients of our food have been absorbed (or so we hope). It’s vital for our health that we are properly eliminating these toxins, otherwise they get reabsorbed into our system. There’s a delicate balance that happens in our body based on fiber consumption, hydration, and muscle motility (determined by healthy brain function) that deter-mines how our bowel movements might appear and how often you’ll pass them.
What Can Your Poo Tell You?
Also known as black caraway and referenced in many scriptural texts, black cumin is a flowering plant found throughout Southwest Asia, parts of the Mediterranean and Africa. This magical oil has a long history of use in diverse culinary and medicinal traditions. Black seed oil is extracted from N. sativa seeds, and has been used in medicine for over 2,000 years due to its many therapeutic benefits. The uses for this natural remedy are all-encompassing. It would be a compliment to your arsenal of supplements, ointments, and aides.
In with Black Cumin Seed Oil, Out with Inflammation
In Part 1 of this series we covered cortisol, progesterone, and their relationship. Though the vast majority of hormones are made of protein, both of these are steroid hormones made of cholesterol. Estrogen is another steroid hormone. It is the main female sex hormone, but it also plays an important role in male bodies.
HORMONES 101 Part 2: Estrogen Dominance
Welcome to our hormone series! We hear all the time that people are curious about hormones, but their complexity makes understanding them a bit difficult. Because of this, we wanted to do a multi-part series covering some of our major hormones and how they interact with each other. We’ll start with cortisol and progesterone. Follow along for more!
HORMONES 101 Part 1: Cortisol & Progesterone
Caffeine is the most widely used psychoactive stimulant drug on the planet. It is addictive, so the body and brain begin to rely on the feeling that caffeine can provide. Although there are some benefits to drinking caffeine (most actually come from the polyphenols found in coffee beans or tea leaves), there are also negative side effects. When dealing with autoimmune disease, it’s likely the brain is already in a state of fight or flight and the effect caffeine has on the body will make that stress worse. Caffeine is known to increase the body’s levels of cortisol, “the stress hormone,” which can lead to other health consequences like anxiety, weight gain, depressed mood, lowered beneficial bacteria in the gut, and even diabetes.
Caffeine Percolates Cortisol
T-regulatory (Treg) cells are the police force of our immune system. As their name suggests, Treg cells regulate our body’s immune response by suppressing it when it isn’t needed. They are extremely important in preventing autoimmunity, which occurs when the immune system attacks the body’s own cells.
Can Olive Oil Help Multiple Sclerosis Patients?
RA is an autoimmune condition in which the immune system mistakenly attacks healthy cells. In the case of RA, the immune system targets the joints leading to inflammation and damage. As a result, it is common for people with RA to experience pain, tenderness, and stiffness in their joints. The hand, wrist, and knee joints are especially vulnerable.
Rheumatoid Arthritis: The Interplay Between Food, the Gut, and the Immune System
Masks have become so politicized that even physical altercations have broken out regarding their usage. While many see mask-wearing as a decision that affects other people and is therefore not entirely personal, others maintain that everyone should take their health into their own hands.
Masking Your Child’s Immune System
Irritable bowel syndrome is a functional diagnosis that is given to individuals who have chronic gastrointestinal symptoms such as diarrhea and constipation, but no inflammatory diseases are found to be the cause. IBS is a frustrating diagnosis because it is often given by gastroenterologists when there is no known cause of the symptoms. Individuals are often left feeling hopeless because there are no medications for IBS.
Irritable Bowel Syndrome vs. Irritable Bowel Disease
For centuries, women have been making groundbreaking contributions to the field of medicine. Unfortunately for much of history, female scientists have been overlooked or had the credit for their contributions stolen. Since March is National Women’s History Month, we here at Dr. Autoimmune wanted to take a moment to highlight some of these scientists. From creating life-saving treatments to discovering new elements, here are some extraordinary women who made waves in medicine:
Women in Medicine
Numerous credible sources have been discussing the link between current events and the increase in autoimmunity. They claim we are facing a ‘super-epidemic’ of autoimmune disease as a result of both the COVID-19 infections and vaccines. This may sound alarming if you didn’t happen to know that we are already in an autoimmune epidemic in the western world. Over the last 30 years, the instance of autoimmunity has tripled! The number of Americans with autoimmune disease now surpasses the number with heart disease. In fact, the most common autoimmune disease, Hashimoto’s thyroiditis, accounts for 90% of hypothyroidism cases.
The COVID-Immune Connection
‘Gluten’ is a word that most of us in this day and age are familiar with. Comedians love the subject, bakeries proudly offer gluten free options, and the label ‘gluten-free’ is greatly sought after. Gluten is a protein found in wheat, barley, and rye. We all knew whole wheat products as being a part of the food pyramid and a staple of our diets, yet now we are being told to be wary of it- why is this?
Why should you ditch gluten?
Coconuts are not nuts to many people’s surprise, which is an amazing gift to those embarking on an autoimmune nutrition protocol. During the autoimmune nutrition protocol, nuts and seeds are avoided temporarily to aid digestion and gut healing. The low glycemic coconut meat and water inside contain many healthful macro and micronutrients to support gut healing, fight inflammation and boost immunity.
10 Ways to Use Coconut on the Autoimmune Protocol
(Before reading this post, be sure to check out A Case Study in Autoimmune Disease – Part 2 – Evaluation, where Dr. Ian gives an overview of Molly’s initial test results.)
A Case Study in Autoimmune Disease – Part 3 – Implementing Support
(Before reading this post, be sure to check out A Case Study in Autoimmune Disease – Part 1 – Evaluation, where Dr. Ian gives an overview of Molly’s case and what she presented with initially.)
A Case Study in Autoimmune Disease – Part 2 – Testing
In June 2020, Molly, a pleasant 35-year-old woman, presented to me for an evaluation of a hypothyroid condition. Molly’s symptoms included fatigue, lack of focus, unstable mood, digestion issues, and skin and hair problems. On top of these symptoms, she had a nagging hip injury that prevented her from exercising, her main form of stress relief. She loved life and spending time with her family and husband but had pulled back from social activities and confided in me that her libido had also significantly suffered as a result of her health challenges. She wanted to get healthy enough to have a baby and be the best wife she could be for her loving husband.
A Case Study in Autoimmune Disease – Part 1 – Evaluation
Routine vaccinations have been a part of preventative medicine since the first smallpox vaccine was officially created in 1796 based on African discoveries brought to the west by a slave named Onesimus. Vaccinations used en masse can halt an infectious disease’s spread through herd immunity. This has been shown historically in regards to smallpox, tuberculosis, polio, and typhoid fever, just to name a few (8).
Should you get the vaccine?
There is a phrase in functional medicine by Mehmet Oz: “Your genetics load the gut; your lifestyle pulls the trigger.” Specifically, genetic risk for autoimmunity sets the stage, but our environment (lifestyle, diet, and mindset) can trigger a happy or tragic ending.
How Does Autoimmunity Start?
We’ve always been told that we get vitamin D from sun exposure. Perhaps you’ve heard the common rule that everyone needs 15 minutes of sunlight per day in order to maintain healthy levels of vitamin D. But have you ever wondered why it’s such an important nutrient?
Vitamin D’s Role In The Immune System
When thinking about the immune system and all its workings, T-cells probably don’t come to mind. However, these cells are hugely important in the realm of building up your immune system to outside invaders! They don’t attack just any foreign cells within the body though; they travel throughout the body until they reach the foreign substances they are assigned to.
T-Cells and The Immune Response
Even before the coronavirus spread throughout the nations, mental health and corresponding providers were necessary components of the health system for many people all around the globe. But according to the World Health Organization, approximately two-thirds of people around the world with a mental health issue don’t use the professional treatments available, and mental illness affects nearly one out of every four people.
Covid-19 and Mental Health
At Dr. Autoimmune, we specialize in Metabolic syndrome and other metabolic disorders which may be expressed in the form of increased blood pressure, high blood sugar, weight gain around the waist, and abnormal cholesterol or triglyceride blood levels. Each of these symptoms increases your risk of heart disease, stroke and type 2 diabetes.
Diabetes & Diet
If you’re one of the 14 million+ people in America who are suffering from Hashimoto’s disease, you’re probably wondering what you can do to help improve symptoms and get some relief. Hashimoto’s is a disease where the body produces antibodies to the thyroid gland, and can wreak havoc on the hormones that are crucially needed by the body in order to function properly. Research has shown us that Hashimoto’s is more prominent in women, and is more likely to arise if you already have a pre-existing condition such as lupus, diabetes, Celiac or rheumatoid arthritis, just to name a few.
Hashimoto’s and H. Pylori
When it comes to contraception, there are many different forms of birth control out on the market to choose from. From implants and shots to pills and sterilization, the choices can be overwhelming for those women looking to have a reliable source of contraceptive. According to the Centers for Disease Control and Prevention, over 12% of women between ages 15 and 49 use birth control pills. This hormonal form of birth control is certainly effective; between helping to manage the painful effects of endometriosis to preventing pregnancy and aiding in making periods shorter and less painful, birth control pills can be a popular choice among women of many different stages of life.
Your Thyroid and Birth Control Pills
ADHD (otherwise known as attention deficit disorder) is a non-discriminatory disorder affecting people of every age, gender, IQ, religious and socio-economic background.(1) If you have children who you suspect have atypical neuro behavior, there’s a large chance they inherited from you (most commonly the mother). ADHD, AD/HD, and ADD all refer to the same disorder. The only difference is that some people have hyperactivity and some people don’t. (1)
Adult ADHD/ADD
Allergies are an issue that many of us are familiar with; with over 40 million people experiencing some type of allergic reaction to different substances every day. It is helpful to determine what forms of allergies are out there and the connection between the responses that our bodies have to what has possibly happened early on in life to precipitate those allergies.
Early Life Medications & Allergies
Did you know that when you walk downstairs, the total weight on your knees can reach as high as five times your body weight? The knee is the largest, and most complicated joint in the human body.
A New Approach For Knee Pain
If you’ve got a child that is returning to school, strengthening their immune system is the best defense against any dis-ease! Support your family from immune stress and vulnerability by knowing the facts.
Back to School Immune Support
What you put in your mouth every day sets the stage for how well your body functions, down to fueling the smallest building blocks you don’t necessarily think about as you choose a banana over a baked good.
Feeding Your Stem Cells
Our immune system does much more than guard against colds and flu. Yes, it works to fight germs and harmful bacteria, but it also determines which cells are good and bad. If the immune system is not balanced correctly, it can essentially turn against its own cells, resulting in an autoimmune disease. There are more than 100 autoimmune diseases, and it is estimated up to 8% of people globally are affected by one or more of them.
Vitamin D to Fight Hashimoto’s Disease
We know that incorporating regular sessions of physical activity into your everyday routine is beneficial for health, and in more ways than one; not only can exercise help you lose weight, but it can also reduce anxiety, decrease your risk of certain cancers, reduce the risk of developing diabetes, help to increase balance and coordination, and build strength within the muscles and bones. But did you know that exercise can also help to reduce neurodegeneration that occurs with age?
Exercise & Neurodegeneration
Are you living with shoulder pain? If so, you are in good company, because shoulder pain is extremely common. According to statistics, approximately 26% of the adult population seek care for pain in the shoulder and up to 70% of people will experience clinical shoulder pain in their lifetime.
A Revolutionary Remedy for Shoulder Pain
At Dr. Autoimmune, the tenets of functional medicine inform every consultation about sleep optimization. We work with patients to uncover what might be behind sleep issues and setting goals to achieve an amazing night’s sleep!
Embrace Sleep and Dramatically Improve Your Health
There are still many unanswered questions about the new coronavirus, or COVID-19, and how it affects our bodies once we are exposed. Aside from basic sanitation tips, many are asking their functional medicine doctors if there are ways we can bolster our immune systems to limit the effects of the virus should we contract it. What additions to our diet or supplements can we add that might help?
Coronavirus and Natural Supplementation
Nearly 100 million Americans suffer from chronic disease such as high blood pressure, diabetes and cholesterol problems, and the “pill for the ill” approach of traditional treatment has resulted in skyrocketing healthcare costs with no relief in sight. While diet and exercise prescribed by local medical centers can change the course of chronic disease, finding and addressing the actual cause of an illness or disease, and practicing the “think and link” model of Functional Medicine, promises to improve the overall quality of life for those suffering.
Functional Medicine: What is It?
Since I returned from serving as a Nurse Practitioner on the front lines in NYC over the past month, I have had many requests to share my story. After some time to process my experiences there, now it’s time to share them with you, our Dr. Autoimmune Family.
Report from the COVID-19 Front Lines in NYC
When it comes to pain management for those suffering from autoimmune diseases, much research still needs to be done, especially within the realm of gut microbiome and the role it plays in managing pain and the corresponding symptoms; however, there are some ways that the digestive system and overall immune system can be boosted while also dealing with pain that results from autoimmune diseases!
Autoimmune Patients: Controlling Pain
When it comes to the virus regarded as COVID-19, knowing how it spreads and how to protect against it is key – but, since there are no known treatments for this disease as of yet, it can be helpful to look from a functional medicine point of view to see what natural ways our bodies might fight and protect against the devastating effects of this virus. This respiratory virus presents with symptoms like fever, coughing, and shortness of breath, and is spread through air droplets from person to person.
Functional Medicine and The Fight Against COVID-19
Have you heard the headlines recently? It’s a bit frightening to hear what’s going on in the world, the nation, and our town. In order to make the news, something has to be HUGE ~ violent, frightening, over the top, unthinkable. We have become immune to subtlety. If we don’t get an intense visceral reaction, it’s not doesn’t have an impact. Unfortunately, this creates an elevated sympathetic nervous system response that literally affects our health.
Let Your Health Soar
When you hear the term “coronavirus”, it might elicit some type of fear…but why? Coronaviruses have actually been around for a long time, with the first case being acknowledged back in 1937 in birds and in the 1960’s with humans. These viruses are the cause of what’s known as the common cold in many people – eliciting symptoms such as a sore throat, cough, fever, and runny nose, just to name a few. These viruses can be passed in several ways, like through shaking hands, touching a surface with the virus and then touching your face, or through a cough or sneeze in the air.
Coronavirus and Natural Supplementation - Functional Medicine
When we think about our immune system, we usually jump to colds and flu, but the immune system does so much more than that! Aside from destroying germs and harmful bacteria within the body, the immune system also determines which cells are good and bad. When the immune system isn’t balanced correctly, it can essentially turn against its own cells, resulting in an autoimmune disease.
Hashimoto’s and Vitamin D Supplementation
In regards to the endocrine system, we might not think that certain factors within the environment could cause disruption to the overall function of this system within the body…until they do. Recent studies have shed light on the fact that manmade and environmental toxins and products are increasing the risk of not only problems like cancer and reproductive issues – but they’re also increasing the risk of developing Type 2 diabetes.
Endocrine Disrupters and Type 2 Diabetes
When we think about food, our first thought is probably not how the nutrients within what we’re eating are essentially building blocks for many internal processes that are going on every day in our bodies – even down at a cellular level. Granted, not everything that we consume is healthy…there are plenty of toxic things that can get into our bodies that aren’t helpful at all. However, what you put into your mouth every day can certainly set the stage for how well stem cells within the body grow, proliferate, and even protect against toxins.
What to Eat to Keep Stem Cells Happy
Do you struggle with sleep? Perhaps you have difficulty falling asleep at night, or you wake up throughout the night, and/or you feel chronically exhausted during the day. Or maybe you fall asleep fine and stay asleep, but force yourself to wake up early for certain obligations and therefore lower the total time you sleep per night. No matter the reason, a great amount of Americans find adequate sleep to be elusive. In fact, 40% of American get less than 7 hours of sleep while the recommended number of hours is between 7-9 hours for adults according to the National Sleep Foundation (Jones, 2019).
Beyond Why We Can’t Just Be Getting By on Little Sleep –
With almost 100 million people in the USA suffering from chronic disease (high blood pressure, diabetes, cholesterol problems), health care costs skyrocket. Considering that so many people are affected by a chronic illness, it would make sense to think that determining a way to treat these diseases at the root is ideal – and granted, many of these can have their course changed by diet and exercise. But what if those aren’t enough? How do we delve further into the pillars of health and reverse these chronic conditions? That’s where the functional medicine model of treatment comes into play. <a href="https://jamanetwork.com/journals/jamanetworkopen/fullarticle/2753520?resultClick=1&utm_campaign=Newsletter&utm_source=hs_email&utm_medium=email&utm_content=78827125&_hsenc=p2ANqtz-_1d-jFf4HsaL2z9dS9qYcf5JNM9z6uMJVSTlEPKF23-DnCxsNmrvCR2eX7XeX64_x6FKrdkGiVrRYljqkhMnj_zAdc_Q&_hsmi=78827125">(3)</a>
What is Functional Medicine?
Rheumatoid arthritis (RA) is a crippling autoimmune disease, typically affecting close to 1.5 million people in the United States alone. This inflammatory illness causes joint pain, loss of mobility, and swelling within the body. This occurs because the body’s immune system accidentally ends up attacking itself, and this happens first at the tissues and membranes that surround and protect joints.
Natural Remedies for Conquering Rheumatoid Arthritis
Exosomes are not a typical term you hear every day, especially in relation to stem cells or mental health. However, these tiny sacs within the body are found within our cellular fluid (mainly within the cytoplasm of a cell), and perform a vast amount of important functions in order to keep the body moving as it should – an even more so in regards to how our cells should be functioning.
Exosomes and Dementia: Is There A Correlation?
The research findings and positive outlook on stem cell usage is amazing – these multidimensional cells can transform into many different types of cells and tissues within the body, and therefore be key contributors to present and future medical therapies.
Stem Cells: Regrowth of Cartilage
Rheumatoid arthritis is a fairly common autoimmune disease, with approximately 1.5 million people in the United States affected in some way. Also known as RA, this chronic illness can progress quickly and is able to do major damage to the body if not treated properly and acutely. Essentially, the immune system within the body accidentally attacks joints and cartilage (detected through rheumatoid factor or CCP antibodies), instead of foreign bacteria and viruses that can cause sickness. This attack on the joints causes inflammation, and results in pain. Typically, this damage and irritation to joints is noticed in knees, hands, ankles, and elbows…. however, rheumatoid arthritis has been known to affect other systems within the body as well, such as the respiratory system (including the lungs and airway).
Rheumatoid Arthritis: The Smoking Gun
Stem cells are an amazing component of the human body, since they can replicate themselves and can be used to help rebuild and regenerate old or defective tissues within the body. Stem cells can be obtained from humans in several different ways, but the two we’re going to look at today are those from adults (autologous) and those from infants (non-autologous).
The Difference Between Autologous and Non-Autologous Stem Cells: What You Need to Know
Hip pain is becoming increasingly common. There are a wide number of conditions that can cause hip pain, however they all share certain similarities. Regardless of the underlying cause, hip pain can limit someone’s ability to enjoy life in general. Hip pain is generally exacerbated by walking and other upright activities, pushing people to become increasingly sedentary.
Hip Pain Solved With Stem Cell Therapy
Unfortunately, injuries of the spinal column are not an uncommon thing. Studies have shown that incidences like these happen in up to 80 million people each year. Typically, these accidents are caused by falls, violence with knives or guns, and car accidents, along with arthritis or cancer. Spinal cord injuries can cause damage that interferes with normal functioning of motor skills, as well as sensory perceptions.
Stem Cells: Can They Help Paralysis?
Puberty is an important physiological time in both the male and female roles, mainly due to the major transformations that are going on within the human body. Not only does puberty have an effect on the body physically, but mental, emotional, and social changes happen as well. Most of us probably don’t delve into the details of what actually happens when our bodies go through puberty, but the changes that occur have lifelong implications.
Premature Menstrual Cycles: What Are the Consequences?
At Dr. Autoimmune, we hope to help you gain control of your health once and for all. Instead of taking a pill to mask the symptoms of your chronic health problem(s), we deeply explore the root cause of your health issues in order to rehabilitate your health, and then prepare your body to take whatever life throws at it and soar. LiveO2 (exercising while breathing in 100% oxygen) is just one of the extraordinarily effective therapies we have in office that not only helps you heal from any current health concerns and bring you back to baseline, but it also works to take your body and brain far beyond “normal” allowing you to live your most optimal and vivacious life.
LiveO2:: What is it?
Are you living with shoulder pain? If so, you are in good company. According to statistics, approximately 26% of the adult population seek care for pain in the shoulder and up to 70% of people will experience clinical shoulder pain in their lifetime. This makes shoulder pain the third most common complaint in musculoskeletal clinical setting. There is a large number of potential causes of shoulder pain and they are diverse; from postural issues to gallbladder inflammation to cardiac issues, a thorough history and physical examination are vital to correctly addressing the root cause of the problem.
Are you living with shoulder pain?
The most prevalent autoimmune disorder experienced by approximately 30 million of the United States population today is called Hashimoto’s hypothyroidism; this particular disease targets the thyroid gland, and presents more frequently in women than in men. Over time, Hashimoto’s eventually causes the thyroid gland to stop working properly, and can even lead to certain types of thyroid cancer. The thyroid glands are located right below the cricoid cartilage AKA “Adam’s apple”, and is shaped like a butterfly. When hormones are released from the thyroid glands, they contribute to things like helping our brain and muscles work correctly, and also helps us maintain our body temperature.
Hashimoto’s and Hypothyroidism: Natural Therapeutic Management
Discovered as early as 1743, Peyronie’s disease affects men anywhere from 30-90 years of age, and presents itself as a curve or deformation of the penis while erect, along with hardened skin within the shaft of the penis. At times, this disease also correlates with erectile dysfunction, causing pain and discomfort to those affected. A study performed over a span of 35 years showed that the average age that men tend to develop this particular disease is 53 years of age; and, playing a big role in Peyronie’s disease is the occurrence of erectile dysfunction, which correlates with approximately 30% percent of cases.
Peyronie’s Disease: What Is It, and How Can Shockwave Therapy Help?
According to the Centers for Disease Control, almost 25% of people in the United States suffer from arthritis. This ends up being close to 54 million people that are dealing with aches, pains, and swelling in their joints on a regular basis. About half of the people dealing with arthritis within the United States have their work, daily activities, and hobbies limited due to the results of these aches and pains, which is a huge statistic!
Suffer from Arthritis? Stem Cells Can Help.
Allergies are an issue that many of us are familiar with; with over 40 million people experiencing some type of allergic reaction to different substances every day, it’s helpful to determine what forms of allergies are out there, and the connection between the responses that our bodies have to what has possibly happened early on in life to precipitate those allergies. Allergic reactions can happen at any time and to anyone; some of the possible allergens that we’re exposed to today include: latex, dust, pet dander, food, bug bites, drugs, grass, and mold, just to name a few. <a href="https://acaai.org/allergies/types">(1)</a>
Antibiotics and Acid Blockers: A Link to Allergies?
Did you know that when you walk down stairs, the load on your knees can reach as high as five times your body weight? The knee is the largest, and most complicated joint in the human body. Here is a brief study in knee anatomy:
Knee Pain
Here at Dr. Autoimmune, we not only offer Chiropractic, Nutritional, and Neurological rehabilitation, but we also have therapeutic equipment that permit a unique, more natural mechanism of healing the body. These therapies work to treat the underlying cause of an issue, rather than merely treating the symptoms. In office, we offer Cold Laser therapy, Pulsed Electromagnetic Frequency (PeMF) therapy, LivO₂, Back on Trac traction, and Vibration Plate.
PMF Therapy (Pulsed Electromagnetic Frequency)
As a functional medicine nutritionist, there is a lot I want to share with you about the big picture of bone broth and gut health. Not all that we have heard is inaccurate, but there are some fine details that could benefit those who are on the verge of quitting, those who have been struggling with autoimmune conditions for years, or those who feel like they have been eating as well as they could but are still not getting the results. Let us dive into the difference between bone broth and meat stock.
Bone Broth vs. Meat Stock: How to Get the Most Gut Healing
Anyone who has had joint pain will tell you that it is no laughing matter. The limitations that joint pain can place on one’s daily life can vary from minor to severe. If left unchecked, many cases of joint pain will continue to progress into a condition known as osteoarthritis (OA). OA is the most common form of arthritis, affecting over 30 million people in the US it is the leading cause of disability among US adults. According to recent estimates, 1 in 2 people will develop OA of the knee during their lifetime; in obese patients, this risk rises to 2 in 3!!!
Alleviating Joint Pain With Stem Cell Therapy
Here at Dr. Autoimmune, we not only offer Chiropractic, Nutritional, and Neurological rehabilitation, but we also have therapeutic equipment that permit a unique, more natural mechanism of healing the body. These therapies work to treat the underlying cause of an issue, rather than merely treating the symptoms. In office, we offer Cold Laser therapy, Pulsed Electromagnetic Frequency (PeMF) therapy, LivO₂, Back on Trac traction, and Vibration Plate.
Who, what, when, where, & why of Cold Laser Therapy
Balloon Sinuplasty is a safe, effective, and minimally invasive technique used to treat blocked and/or inflamed sinuses. Sinuses can become inflamed from a variety of conditions, such as sinusitis (sinus infection), other chronic infections, and can even result from mold exposure (MARCoNS). This endoscopic, catheter-based technique is an alternative to sinus surgery and can be beneficial for patients who are not responding to medications for relief of their symptoms. Furthermore, balloon sinuplasty does not require incisions, cutting, the removal of any bone tissue, or anesthesia and is therefore less taxing on the patient.
What is Balloon Sinuplasty?
Many people just like you are feeling the aches and pains of old age. But are these aches and pains normal? Just because it is common doesn’t mean you have to embrace inflammation and deterioration of your body. Just imagine growing old and still feeling your youthful, agile body move with ease. Doesn’t this sound like a dream? Well, it doesn’t have to be just a dream. You can live a life with less pain and more resilience. With a functional approach to your health your body doesn’t have to be subject to arthritis.
The Functional Medicine Approach to Arthritis and Why It Works
Lasers, powerful beams of light that affect how our body functions whether it’s our eyes, our fat cells, and now research is showing our thyroid. In 2015, I wrote a blog about low level laser therapy and the thyroid based in research out of Brasil.
Autoimmune & Lasers: The future is now!
Until recently, we thought there were only two types of diabetes – Type 1 and Type 2. Now we have come to learn that there is another ~ Type 3 Diabetes. Type 1 is an autoimmune condition seen typically in young children whereas Type 2 is a lifestyle disease due to unhealthy choices that leads to insulin resistance and high blood sugar. Type 2 has also been referred to as “adult onset” diabetes, although children are now developing Type 2 Diabetes due to poor diet and a sedate lifestyle. The symptoms of Type 3 Diabetes affects the brain specifically. It has another name you may be more familiar with ~ Alzheimer’s disease.Type 3 Diabetes marks the progression from Type 2 Diabetes to Alzheimer’s disease and other forms of dementia. A dramatic decline in cognitive function and marked memory deficits highlight the key symptoms of Type 3 Diabetes.We can clearly see that your pancreas is not the only organ that changes function due to high blood sugar levels. Instead of just having insulin resistance in the muscle, liver, and fat cells, we can develop insulin resistance in the brain.
Diabetes and Alzheimer’s – the connection no one’s talking about.
My name is Dr. Henry Zaremba DC. Working at Dr. Autoimmune has been a dream come true for me! I am excited to be a part of the cutting-edge healthcare that is being provided in this practice. I want to focus on one particular aspect of our practice: Functional Neurology. I thought I would take this opportunity to define what functional neurology is, as well as the principles that shape it.
Functional Neurology: the who, what, when, where, & why – With Dr. Henry DC
Do you suspect you have a thyroid condition or maybe you know for certain? You have terrible fatigue, constipation, cold feet or hands, hair and skin problems, weight fluctuation, and brain fog that don’t seem to be getting any better despite eating well, sleeping, and trying to focus on what you’re doing. You are one of the 40 million Americans who suffer from Hypothyroidism! But is it really just a simple thyroid problem or is there more to the story?
Healthy Gut, Heathy Thyroid – The Unacknowledged connection.
Posttraumatic Stress Disorder or PTSD is a type of psychiatric disorder that develops after witnessing or experiencing a traumatic event. It can be as vivid as war and major disasters or as subtle as a being abandoned or alone in a time of need. It can happen to anyone, at any age and it affects 3.5% of adults in the United States.
PTSD, the monster within.
ASD or autism spectrum disorder is a type of developmental disorder, which affects behavior and communication. Though patients suffering from autism may get diagnosed from the disorder at any age; but, it is considered a developmental disorder as its symptoms appear during the initial two years of a child’s life. The Diagnostic and Statistical Manual of Mental Disorders (DSM-5), which is a guide used in the diagnosis of mental disorders, states that people suffering from ASD have the following:
Autism Spectrum Disorder: the who, what, when, where, & why.
Autoimmune disorders occur when the immune system malfunctions. That is, instead of helping protect you against infections; it attacks your own tissues and organs. Scientists are not clear on what exactly causes an autoimmune disorder; however, multiple factors like genetics, environment and triggers play a significant role.
Autoimmune Diseases & the Infection Connection
Hashimoto’s thyroiditis is an autoimmune disorder in which the immune system of the body attacks the thyroid gland, a gland which is located beneath the Adam’s apple in your neck. This gland forms a part of the endocrine system of the body which secretes various hormones to coordinate multiple functions of the human body.
I felt a great disturbance in the microbiome…
Unlike other camps, ours is individualized to meet your child’s specific needs and the times are flexible to meet your schedule! The brain is highly complex and that’s why we’ve created a program to identify key areas of weakness and use specific tools to develop those areas. The results can be life changing!
Brain Camp for Children & Young Adults #2
Brain Camp is an integrated approach to supporting families unique goals for their children. Whether your goal is to improve the function of a child with Autism or ADHD or improve your child’s ability to thrive in life and school, this camp is focused on supporting your child to be his/her best!
Brain Camp for Children and Young Adults
The flu can be miserable! Do you stress whether or not you should get the flu vaccine every year? Or do you wonder is it worth it? It’s a hot topic and if you just look at the numbers you may not be seeing the full picture. Not to trivialize how awful it feels to have the flu, but the reality is the data from the Centers for Disease Control (CDC) is a horror show of conflict and political nonsense. In this article, I hope to clear up some of the fear-mongering used from statistics collected by the CDC and give you action steps to help naturally prevent the flu in the coming years.
Is It All A FLU(KE)?
If you’re struggling with one or both of these conditions please take the time to watch the latest webinar covering Dr. Autoimmune’s Functional Medicine approach to taking on Anxiety and/or Depression featuring Dr. Ian Hollaman, DC, MSc, IFMCP.
Anxiety, Depression, Relief! – FREE Webinar & Brain Balancing Handout
It can be incredibly confusing and frustrating for anyone suffering from thyroid symptoms to go for years if not decades without a proper diagnosis. Did you know that 95% of people with thyroid disease have a history of a gastrointestinal disorder called “leaky gut” that is the precursor to the body producing antibodies against their thyroid? As these antibodies form and bind to the thyroid they slowly start to destroy the thyroid, which eventually impacts the ability to make thyroid hormones. This is why TSH eventually goes up although it can take decades. Although it may be a relief to finally get a diagnosis, the common medications do not stop the disease from destroying the thyroid and medications frequently need to be adjusted. If you have a thyroid disease, it is most likely auto-immune in nature. As a result, the immune system needs to be addressed in order to truly address the underlying causes of your thyroid disease. Supporting your triggers, genetics, and environment through a customized approach is essential to regaining your health!
Top 10 Thyroid Myths Revealed!
We used to think there were two types of diabetes – the type young children contract (Type 1 – Autoimmune) and the type you get that is brought on by a combination of unhealthy lifestyle choices, called (Type 2), or adult-onset diabetes.
Diabetes and the progression to Alzheimer’s
If you are interested in learning more about Thyroid Conditions OR Red Tail Wellness Centers’ Functional Medicine approach: I encourage you to come to our next Functional Medicine Seminar. There is no cost nor obligation AND attendees will be invited to enjoy exclusive, new patient pricing (Bio-Impedance Analysis, Metabolic Exam, Case Review, AND Care Recommendations for only $175 – regularly priced at $475). What you learn will open your eyes and mind to a bright and healthy future. Limited seating, call to reserve your seat today 303.882.8447 OR register online through the form below!
The 10-step Thyroid detox.
Did you know that insulin resistance and pre-diabetes are precursors to diabetes? That means that there are warning signs that your body gives before it develops the disease. The question is, did your doctor make you aware of the warning signs and were you given the appropriate tools to reverse the signs? Type 2 and type 3 diabetes are complex metabolic disorders – yes, metabolic, not genetic. That means they are diseases of lifestyle. Therefore, if your lifestyle changes, your health changes. How empowering is that!?! You don’t have to live in fear of losing a limb, going blind, developing neuropathy, or even Alzheimer’s disease as in type 3 diabetes.
Insulin Resistance – Diabetes & Pre-Diabetes
During my lectures to patients and doctors, I try to stress that the endocrine system is like a well-tuned machine, always getting feedback from various data points and making adjustments so that we can continue without a major break down. But, as is the case for the 40 million plus Americans who suffer from Thyroid disease, when things do break down, we rely on a technician that may not have a full understanding of the different systems that influence thyroid health. If you complain of weight gain, fatigue, constipation, brain fog, cold feet, and hands or your hair falling out, then more than likely a medical doctor will run a TSH blood sample (thyroid stimulating hormone) to determine if your thyroid is working appropriately.
Thyroid Health – 10 Reasons why people struggle to improve their health (+1 HUGE bonus)

The Functional Medicine solution to a Pain in the Gut
If you’re interested in learning more about how our Functional Medicine approach can help ease your Thyroid condition symptoms:
Leaving your Thyroid symptoms in the dust!
“I feel like this depression is a never ending story. Will I ever get better and feel good, happy and healthy again? I can’t take this anymore. It keeps pulling me down into the blackness and I wish with all my heart I could take it away. I’m tired, so tired of this constant battle. I want to feel like me again. I used to be so happy. I used to sleep through the night and feel energetic all day. I didn’t use to live with all this pain”.
Depression/Anxiety and the Brain-Gut connection
Support ADD / ADHD, sensory integration disorders, and other learning and behavioral conditions with a non-drug approach called Neurofeedback.
ADD / ADHD Lecture: A Non-Drug Approach | April 27th
($750 Value – Expires June 1st, 2017)
Neurofeedback Special – Alternative Therapy for ADD/ADHD
Call (303) 882-8447 or use the form below to learn more and schedule your exam.
Help for Knee Pain – Special Offer on Exam and Report of Findings
Dr. Autoimmune presents a Thyroid Health Happy Hour with a screening of the docuseries The Thyroid Secret on March 14th at Shine Restaurant in downtown Boulder.
Thyroid Health Happy Hour – March 14th at Shine Healing Thyroid Tissue with Cold Laser & without Medication
Healing Thyroid Tissue with Cold Laser & without Medication
Thursday, January 26th • 6pm • at our North Boulder Office
Digestive Health Lecture – January 26th
My friend Dr. Izabella Wentz and her amazing team have put together an <strong>incredible 9-part documentary series on thyroid disease</strong> that’s going to be nothing short of groundbreaking when it comes to how we treat one of the most overlooked diseases in our country today. And the buzz is already building around this powerful documentary series that Izabella and her team have produced.
Dr. Ian to be featured in a Thyroid docu-series
Wednesday, January 18th • 6pm • at our North Boulder Office
Thyroid Lecture – January 18th
Community Supported Agriculture, also known as CSAs or farm shares, has become an effective way for people to buy local, seasonal, organic food directly from a farmer. It’s a simple, community-building idea that has had a positive impact on communities and farmers alike. It also makes local, organic, seasonal foods accessible to many, and adds significant nutritional value to the diet. Because of the natural and soil-building practices of organic and biodynamic farms, the food produced on these farms can have much more nutrition than produce from a store.
Why buy a farm share & which one to choose
A new research study links birth control usage, especially in teens, to a significantly higher risk of clinical depression. The September article, published in JAMA Psychiatry, confirms what many women have suspected for years – I’m not crazy and these pills are making me sad! Specifically, researchers studied over one million women from 1995 to 2013 and found that women using all types of hormonal contraception were associated with increased risk of depression and use of anti-depressants.
New study links birth control pills to depression – “It really isn’t in your head”
The thyroid gland regulates the body’s metabolic system and plays an extremely important role in human health. Because all cells require thyroid hormone for proper functioning, thyroid disruption can have a wide range of effects on virtually every system of the body. Chemicals that interfere with thyroid function must be treated with great caution. There is <a href="http://www.fluoridealert.org/studies/nrc_thyroid/" title="" target="_blank">substantial evidence</a> that fluoride exposure can impact thyroid function in some individuals.
Dangers of Fluoridated Tap Water & it’s Connection to Low Thyroid Function
1. **Gluten Intolerance –** I know this may be in the “DUH” category for many educated autoimmune disease sufferers but what most doctors don’t know is that it is not just Celiac disease that can cause the activation of pro-inflammatory genes. Dr. Aristo Vojdani over at Cyrex labs changed the game forever when he released their <a href="https://www.cyrexlabs.com/CyrexTestsArrays/tabid/136/Default.aspx" title="" target="_blank">panel #3</a>, which includes 24 antibodies that your body may produce against gluten, wheat, wheat germ, etc. If you are going to get screened for gluten intolerance or Celiac disease, please be thorough (and no, insurance doesn’t cover it)!
10 causes of autoimmune disease your doctor may not know about!
**Feeling Inspired to Create Change?**
Hashimoto’s Awareness & The Top Ten Weak Links In Hashimoto’s Thyroiditis
So you were diagnosed with a thyroid condition or you suspect you have thyroid disease because you have constipation, cold feet or hands, hair and skin problems, terrible fatigue, weight gain and brain fog? Well, join the 40 million other Americans who suffer from Hypothyroidism. But is it really just a simple thyroid problem? Do you suspect there is something more going on below the surface that has the thyroid entangled?
The Thyroid Gut Connection
**Proton pump inhibitors and chronic kidney disease – what you need to know!**
Healing Acid Reflux Naturally
I think a big take home for my auto-immune clients is to realize the complexity of the immune problem requires a comprehensive approach to reestablish optimal health. The first task at hand in supporting autoimmune diseases like Hashimoto’s is to completely heal intestinal hyperpermeability, also known as leaky gut. This requires multiple months of a low allergen diet (5R, elimination/provocation) plus supplementation specific to your needs. Secondly the thyroid itself is inflamed. Just because you help the gut heal does not mean the thyroid automatically heals from the relentless attacks by your immune system. This is where altering glutathione levels and using protocols like pulsed electro magnetic frequency therapy and <a href="https://redtailhealth.com/can-laser-help-your-thyroid/" title="" target="_blank">low-level laser therapy</a> to the tissue can make a big difference. This typically takes 16-20 sessions to make a considerable difference in the healing process. Lastly, the immune system must be rehabilitated and calmed as it has been functioning in overdrive and has been acclimated to drive autoimmune attacks against your tissues. This is where _immunomodulation_ becomes critical to optimize function. I personally use a specific protocol of supplementation, diet and lifestyle changes that promote regulation of the immune system and tolerance to your tissues. If all three of these critical factors are put into place then the body truly has a chance to heal itself and you most likely will start to feel like a human again! But, be prepared to work for 6-12 months. Changes do come faster than this thankfully but if you are dedicated and committed to that change then you may be a good fit at Dr. Autoimmune.
The iodine & selenium debate – how much is enough for the thyroid?
The typical person with Hashimoto’s Disease is female, although men can have Hashimoto’s. The development of symptoms are usually associated with a significant hormonal fluctuation such as pregnancy or a period of stress. Symptoms such as low energy/fatigue, hair loss, depression/anxiety, constipation, cold hands and feet, heart palpitations, increase in weight even though they may not be excessively consuming calories, and mental sluggishness (brain fog) are some of the most common complaints. Sounds familiar? Then blood is pulled and hopefully the TSH level is elevated (_people can still have all of the symptoms and normal TSH because of CAT_) indicating hypothyroidism. Medication is given and the patient is told to take this the rest of their life, regardless if they continue to have symptoms after hormone replacement!
Can Laser Help Your Thyroid?
ADD/ADHD spectrum disorders are often thought of as strictly brain related. In fact, that is often what gets addressed when looking for ways to control the symptoms associated with the diagnoses. However, there is a strong link to what is happening in the brain to what is happening in the gut. According to Dr. Perlmutter, the author of “Grain Brain” and “Brain Maker”, around 6.5 million children are living with a diagnosis of either ADD or ADHD.
The ADD/ADHD Brain And Gut Connection
**Chances are that you have heard the term “neurofeedback” in relation to new techniques being used to help with symptoms of: ADD; anxiety; autism; PTSD; dementia; depression; “brain fog”; insomnia; chronic pain; and other neurologic based conditions. But what is neurofeedback and how does it work?**
Neurofeedback: Training for Your Brain
!<a href="https://redtailhealth.com/wp-content/uploads/2015/05/imgres-1.jpg" title="" target="_blank">imgres-1</a>
New Wellness Book!
!<a href="https://redtailhealth.com/wp-content/uploads/2015/05/cauliflower_brussel-sprouts-272x300.jpg" title="" target="_blank">cauliflower_brussel sprouts</a>
Delicious Detox Recipe: Cauliflower with Roasted Brussel Sprouts
**!<a href="https://redtailhealth.com/wp-content/uploads/2015/05/Thermometer-Warning-300x270.jpg" title="" target="_blank">Thermometer Warning</a>Is this part of why you are not healing?**
Celiac Disease & Mercury Connection – A New Link?
Though America’s health care has become a political battlefield, we the people can be grateful for, among other advantages, our top-notch acute hospital care and our unparalleled ability to guide an injured citizen through a medical crisis. Chronic disease, however, is where we fail miserable so much so, that we’re currently ranked 37th of industrialized nations, yet we spend two times more than the second highest-spending nation.
Functional Medicine: A Health-Care Future Worth Fighting For
Is it true that training leads to better performance and fewer injuries? Vince Lombardi said, – perfect practice makes perfect -, not practice makes perfect. Vince was correct in that proper training far outweighs any quantity of training. So, what is proper training? Proper training focuses on balancing structural, nutritional and emotional health.
Perfect Training = Perfect Performance
“The craniofacial morphology of patients with celiac disease reveals an altered pattern of craniofacial growth,” claims an article titled ”Large Forehead: A Novel Sign of Undiagnosed Celiac Disease,“ in a 2005 issue of Digestive and Liver Disease.
Is Your Forehead Related to Your Irritable Bowel Syndrome?
Do you cringe when asked about your cholesterol? The word alone strikes fear of atherosclerosis, heart disease, and stroke. All the studies, the diets, the doctors’ orders seem geared toward lowering cholesterol, eliminating the “bad” kind, and consuming low-fat, cholesterol-free foods. Interestingly, there is little scientific evidence showing that cholesterol is a cause of atherosclerosis, heart disease, or stroke. Rather, current research indicates that cholesterol actually protects against these diseases and many others.
Cholesterol: A Love Story
!<a href="https://redtailhealth.com/wp-content/uploads/2015/04/SignLanguage.jpg" title="" target="_blank">SignLanguage</a>“Cold hands, warm heart” a sweet old adage that may say more about the thyroid than the personality. Anxiety, depression, fatigue, digestive troubles, constipation, insomnia, heart palpitations, itchy dry skin, brittle thinning hair, difficulty with weight gain or loss, morning headaches, cold hands and feet are the signs of a poorly functioning thyroid.
Thyroid Sign Language
!<a href="https://redtailhealth.com/wp-content/uploads/2015/04/DentalExam.jpg" title="" target="_blank">DentalExam</a>Most of us understand that Mercury is a toxic metal that can cause serious health concerns. Besides an old broken thermometer or vaccination, what is the most common way we are exposed to harmful levels of mercury? The answer is to look at your teeth!
Mercury & Your Thyroid: How Many Fillings Do You Have?
!<a href="https://redtailhealth.com/wp-content/uploads/2015/04/toast.jpg" title="" target="_blank">toast</a>I had the pleasure to present “Nutritional Repercussions of Celiac Disease” to the Boulder County Celiac Association this past August. Celiac Disease and gluten intolerance are very important to me, as I was diagnosed gluten intolerant during a stressful period in Chiropractic College and my grandfather suffered from Parkinson’s disease brought on as a complication from Celiac Disease. Although gluten is becoming a household word, many people including doctors are not aware of the complexity and seriousness of being gluten intolerant or Celiac. It is my hope that you will gain insight into your condition and be empowered to make changes that will improve your quality of life.
Nutritional Repercussions of Celiac Disease
Most everyone has experienced some form of pain in his life, whether falling off a bicycle, lifting a heavy box, a stress headache, or due to a car accident. All of these different injuries stem from the same response in the body–inflammation.
Inflammation Strategies
**Well, according to the research, YES!!!**
Do Low Carb Diets Promote Weight Loss?
1) The disease does not stop after going gluten free – A 2009 study from the Journal of Alimentary Pharmacology and Therapeutics indicated that after studying 465 Celiac disease patients only 8% of the group reached “histological normalization” after following a strict gluten free diet for 16 months. That is, only 8% of the group regained a healthy gut. Their final conclusion:
5 Things I wish I knew when I was diagnosed gluten intolerant
Have you ever gone through your day feeling like you were in a fog? Or you ate something and then felt like you were dragging through the day? According to Dr. Datis Kharrazian, everything you have ever experienced, felt, or conducted in your life is due to brain function. The ability to enjoy, perceive, sense, and experience life is dictated by the firing of your brain.
Awakening Consciousness Through Healthy Brain Function
**Wrong!** Remember, in the movie Titanic, the panoramic ocean scenes with icebergs dotting the horizon? And the scene where Leonardo DiCaprio, leaning overboard, notices an iceberg suspiciously close on the ship’s starboard side? What happened to the Titanic is what closely resembles our current health-care approach and attitudes toward gluten intolerance and celiac disease. What seems small and insignificant on the surface is actually gigantic and life-altering.
Gluten Intolerance: Solely a Gut Issue, Right?
Hypothyroidism affects approximately 34 million people (11%) in the United States, a majority of those being female. Unfortunately, many people and practitioners don’t recognize hypothyroidism as an autoimmune disease, even though 90% of hypothyroid cases are autoimmune! —– The presence of thyroid antibodies in blood work is conclusive for the autoimmune disease, known as Hashimoto’s. These antibodies gradually and continually destroy the thyroid gland, eventually resulting in thyroid failure. Patients are typically offered thyroid hormone replacement therapy or, alternatively, iodine and glandular supportbut these treatments actually add fuel to the fire!
Hypothyroidism: Treating Fire with Fire???
Vitamin D is a hot topic these days, and for good reason. While it’s importance for bone health has long been known, current research is finding that sub-optimal vitamin D is implicated in many disease states, especially for pregnant women, their unborn children and their nursing infants. That begs the question of what is a healthy amount of vitamin D and is it the same for everyone?
The Hottest Hormone in Medicine: Vitamin D – Is Your Family Getting Enough?
Modern research, including the work of Alessio Fassano, the world’s preeminent researcher in Celiac disease is confirming what has been the suspected cause of autoimmunity – the Gastrointestinal Tract. Gastrointestinal problems can shatter the fine balance of the gut barrier and begin the process of “leakage” of undigested antigenic materials (foods, bacteria, etc) into the sub-mucosa and then bloodstream. The immune system’s job is to identify, tag, then eliminate invaders whether they are infectious or large protein molecules from undigested foods. This process of materials seeping into the circulation challenges the immune system and activates pro-inflammatory cytokines (immune system bullets) and our antibody system, which further exacerbates the intestinal barrier permeability (“leaky gut” syndrome).
Leaky Gut & Chiropractic
As many of you know, Dr. Karen, Cecelia, and myself are gluten free. It’s not just because we’re in Boulder, it’s because we both have a family history of gluten sensitivity, we both have serious reactions to gluten, and we know the serious repercussions of consuming this indigestible “food”.
Gluten Free – Just Another Fad Diet?
Many people suffering from either of these conditions may see a close overlap of symptoms, or may have been diagnosed with one and are curious if they have the other. In a 2012 article in Rheumatology International, scientists asked the question: “Does thyroid autoimmunity represent a predisposition for the development of fibromyalgia (FM)?
Is it Fibromyalgia or Thyroid?
Have you ever wondered why going gluten free hasn’t solved your problems? You may know to avoid gluten if you have the autoimmune disorder Celiac disease, but did you know current research indicates going gluten free will not solve all of your problems?
Gluten free but not symptom free?
A study released in January through the Journal of Clinical Endocrinology Metabolism found that Hashimoto’s patients with atypical celiac disease (i.e., no digestive complaints but + antibodies) required 49% more thyroxine (T4) to achieve the same TSH levels as non-celiac Hashimoto’s patients. After following a dedicated gluten free diet (GF) for 11 months their TSH levels dropped precipitously and hovered near the same thyroxine requirement as the non-celiac Hashimoto’s patients.
Should you be gluten free if you suffer from hypothyroidism?
Many of us have heard about the chemical BPA (Bisphenol-A) which is a compound used in the manufacturing process of plastics, and is also found in the lining of cans (and some of you may know it because plastics now advertise “BPA free”). It has been in the news a lot lately because of its association with heart disease, cancer and an array of other long-term health problems. BPA is an endocrine disruptor, which mimics estrogen in our bodies. In a recent study scientists showed that a single exposure to BPA can increase blood pressure within a couple of hours.
Plastics & Your Health – Hypertension Risk?
Although spring is trying to get a start, Colorado tends to be slow on the up take. This month’s newsletter has three information packed articles on anxiety, autism and massage cupping to help you get your spring moving! It is Autism awareness month and recently the CDC just revised their disease incidence figures from 1:80 > 1:50! Dr. Karen speaks on epigenetics and how we can treat, and successfully manage autism, but more importantly how we can PREVENT Autism through mom’s health. Dr. Ian speaks on the most common neuropsychiatric condition in the USA, anxiety. Many are unaware how complex anxiety can be but also how effective it can be treated through the functional medicine model and strategies like heart math training. Lastly, Erin Stanley, LMT, explains how cupping technique can effectively address dysfunction and pain to leave you relaxed and energized!
Autism Awareness, Anxiety and Cupping
Many of you are aware that two of the most common clinical conditions we treat at Dr. Autoimmune is ADHD and autoimmune thyroiditis, or commonly know as Hashimoto’s. An interesting article came across my desk recently when I was wondering how mom’s health could effect the future health of her unborn fetus.
Thyrotoxinemia & ADHD
You are pretty lucky if you are reading this newsletter because the chances that your long term health will be better than most is quite good. That’s because Dr. Ian and I address a little known but devastating condition commonly known as leaky gut. As you may know, a leaky is a GI tract that is not functioning properly. Foods are not absorbed properly, flora and fauna are not balanced, and many unpleasant health conditions can result.
Pediatric Leaky gut – Could this be holding your child back?
Probiotics – Fad or Fabulous? Dr. Ian attains his IFMCP! Dr. Autoimmune turns 5!
Probiotics – Fad or Fabulous?
Have you ever wondered why going gluten free hasn’t solved your problems? You may know to avoid gluten if you have the autoimmune disorder Celiac disease, but did you know current research indicates going gluten free will not solve all of your problems? The single most important aspect of celiac and gluten sensitivity is a gluten free diet.
Have You Ever Felt Going Gluten Free Did Not Change Your Health?
Whenever we talk to people about Neurofeedback, their first question always is “what the heck is that?”. After explaining that Neurofeedback is a simple therapy that helps train the brain to function better, this opens up a flood of fun questions like: “how does it work? what types of conditions can it help? what is the treatment process like?” and most importantly “can it help me?”
ADHD & Neurofeedback
Well, then you can join the millions of Americans who may have been diagnosed with hypothyroidism (not necessarily Hashimoto’s) but still suffer needlessly! One of my goals is to teach about the most common reasons people continue to suffer with hypothyroidism. Below are my top ten reasons:
Top 10 Reasons Thyroid Patients Fail To Heal
Glyphosphate is the active ingredient found in the pesticide roundup. It is considered broad spectrum and non-toxic to humans (Williams, 2000). Recently, that assertion has come into question with a recent paper indicating glyphosphate may be implicated in Celiac, Autism, obesity, neurodegenerative conditions like Alzheimer’s and Parkinson’s, infertility, cancer and depression (Samsel, 2013). Specifically, the authors found glyphosphate suppresses 5-enolpyr-uvylshikimic acid-3-phosphate synthase (EPSP), which is the rate-limiting step for aromatic amino acids in the shikimate pathway of bacteria, plants and archaea. Glyphosphate appears to disrupt gut bacteria in mammals and allow a pathogenic overgrowth to occur. Also, glyphosphate may cause chelation of minerals like cobalt and iron plus suppress cytochrome P450 enzymes. Glyphosphates link with gluten intolerance appears to stem from its affects on the digestive system. Fish exposed with glyphosphate showed tremendous stress on their digestive systems and specifically the activity of amylase, proteases and lipases were inhibited in the esophagus, stomach and intestines (Senapati et al., 2009).
Gluten Intolerance linked to Pesticides?
!<a href="https://redtailhealth.com/wp-content/uploads/2015/04/Coaching_original.jpg--300x201.jpg" title="" target="_blank">Coaching_original.jpg+</a>Many of my clients want that smoking bullet to help them treat and heal their particular concern, be it Hashimoto’s, Celiac, MS, Rheumatoid, Lupus or other disease. We have been trained, just as our medical doctors were trained to associate a symptom with a particular pill or surgery that will magically “wipe away our problem”. Unfortunately with autoimmune disease you cannot get a “new” immune system and you must develop strategies to help the only immune system you have become more tolerant to your tissues (I’m not saying you cannot have an AMAZING life here!). So why would you develop an autoimmune disease in the first place?
Coaching our immune systems towards vitality